Author: Linda Lam
25% of the population manifests anisocoria as a normal, routine examination finding. The hallmark sign in lesions of the pupillary efferent pathways is anisocoria.
Changing consulting room illumination helps to differentiate between physiological and pathological cases.
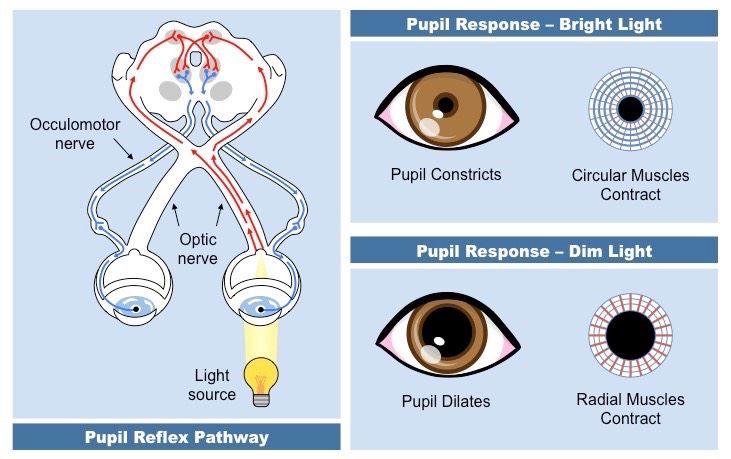
Always test both light and near reflexes and test for a relative afferent pupil defect (RAPD). If an RAPD is present it indicates a problem with the optic nerve.
A quick refresher on some differentials to consider when it comes to pupil reaction:
- Adie’s tonic pupil: post-ganglionic interruption to parasympathetic input to the sphincter pupillae and the ciliary muscle resulting in an internal ophthalmoplegia. Typically in young adult females. Supersensitive to weak pilocarpine (0.1%). No ptosis or motility detected.
- Horner’s Syndrome: due to a compromise of the sympathetic pathway from the brainstem to the eye. It may be described as pre-ganglionic or post-ganglionic depending on whether the causative lesion is situated prior to or beyond the superior cervical ganglion. The affected pupil is smaller with ipsilateral ptosis. If heterochromia is observed it suggests a congential lesion. Reaction to light is normal. Pharmocological evaluation is performed with apraclonidine 0.5% or 1% phenylephrine.
- 3rd nerve palsy: The patient can present with ptosis, eye diverged, no accommodation, pupil dilated and fixed. If acute suspect an aneurysm if the pupil is dilated, ischemia if the pupil is spared. This is a medical emergency and the patient requires immediate imaging
Pupils are quick and easy to assess and should be done routinely. A thorough case history is also vital in determining acute or chronic cases, especially if the patient has had head trauma in the past.